Centers for Medicare and Medicaid Innovation Center: Equity and Vision
Sheppard Health Law
OCTOBER 27, 2021
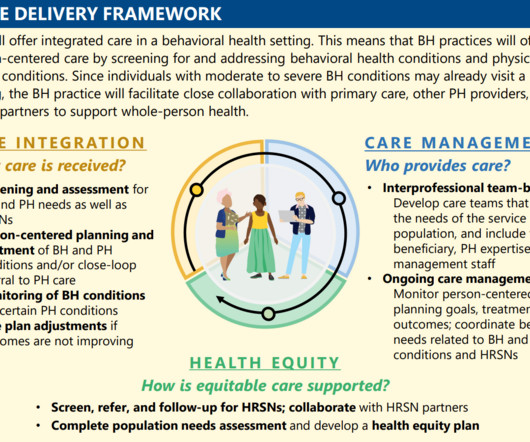
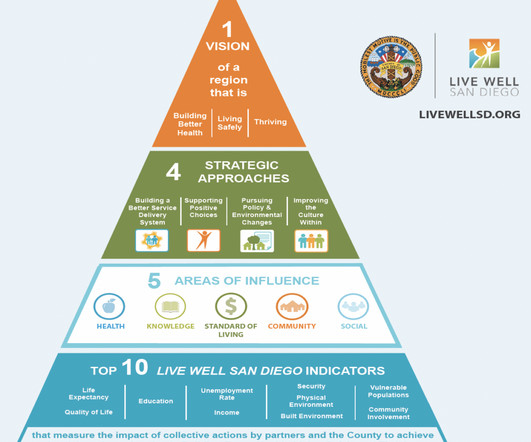
On October 20, 2021, the Centers for Medicare and Medicaid (“ CMS ”) Innovation Center (“ Innovation Center ”) published a white paper detailing its vision for the next ten years: a health system that achieves equitable outcomes through high quality, affordable, person-centered care.














Let's personalize your content