With Medicaid Access Rule Finalized, Home Care Providers Enter ‘Wait-And-See’ Mode
Home Health Care
APRIL 23, 2024
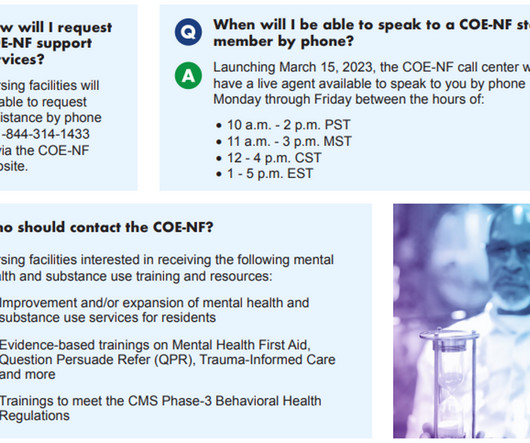
This article is a part of your HHCN+ Membership On Tuesday, Centers for Medicare & Medicaid Services (CMS) officials vehemently backed the thought process behind the “80-20” wage mandate in home- and community-based services (HCBS). In that case, access to care will be directly and negatively impacted.































Let's personalize your content